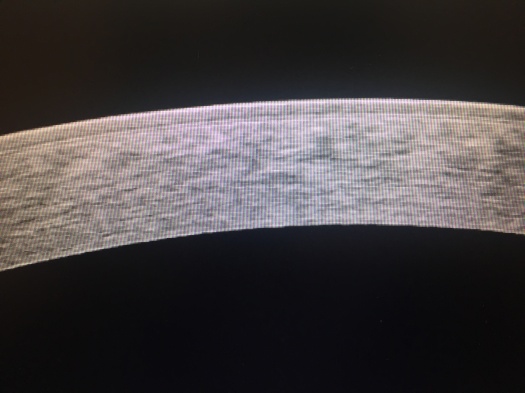
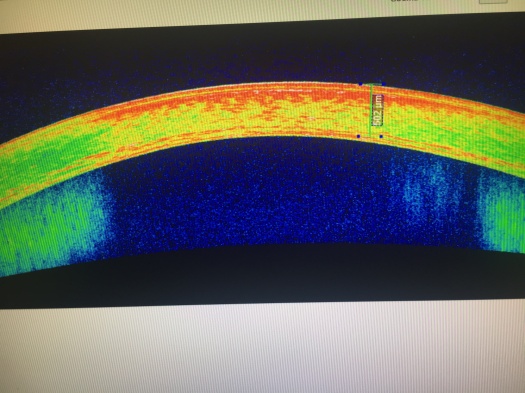
What is Pellucid Marginal Corneal Degeneration (PMD)? In short it is an eye disease very similar to Keratoconus in that it also causes thinning of the corneas. The difference between Keratoconus and Pellucid Marginal Corneal Degeneration is that PMD causes a crescent shaped band of thinning in the lower region of the eye, while the central cornea is usually of a normal thickness; as well as the cornea appearing transparent in PMD . There is a third disease called Keratoglobus that like the previous two also causes corneal thinning (more about this disease will be discussed in a future post).
Now you may ask if there is an actual difference between Keratoconus and PMD and Keratoglobus or if the three diseases are the same. The answer is that doctors are not sure either. They do not know if the three eye diseases are different diseases, or just different phenotypic (expression) variations of one disease.
Some of the different signs of PMD may include drastically reduced uncorrected visual acuity that usually cannot be improved with glasses (usually for astigmatism), roughly normal pinhole visual acuity, and refraction/keratometry that shows against the rule astigmatism (where the astigmatism on a corneal topography is seen horizontally).
Patients are also commonly asymptomatic except for the gradual worsening of vision that is unaided by glasses. The clinical diagnosis for PMD is the same as Keratoconus where the patient is examined by doctor on a slit lamp microscope and checked with patient’s history and supported by corneal topography & pachymetry.